
by Dr. Jacqueline S. Allen | Aug 19, 2019 | Blog, Dental Implants, Dentistry, Endodontics, Endodontist
Risk management is a key part of our everyday lives. When it comes to managing dental health, patients want to be sure that a recommended procedure is safe as well as effective. In the past couple of decades, dental implants have become a popular option for replacing missing or failing teeth. Many people, though, question whether implants are the best choice for their oral health challenges.
While dental implants are not the right choice for every individual, they are in many cases a safe, effective restoration. Their record for safety extends beyond the immediate period after the implantation and has been well-documented for patients with a variety of oral health situations.

Factors That Make Dental Implants A Safe Choice
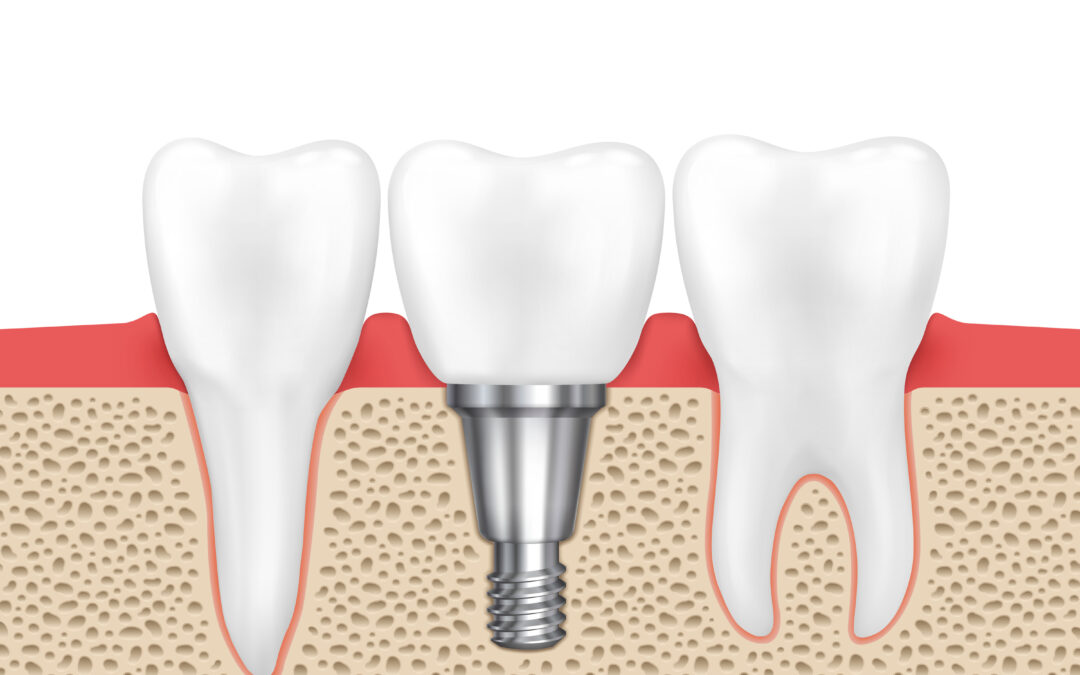
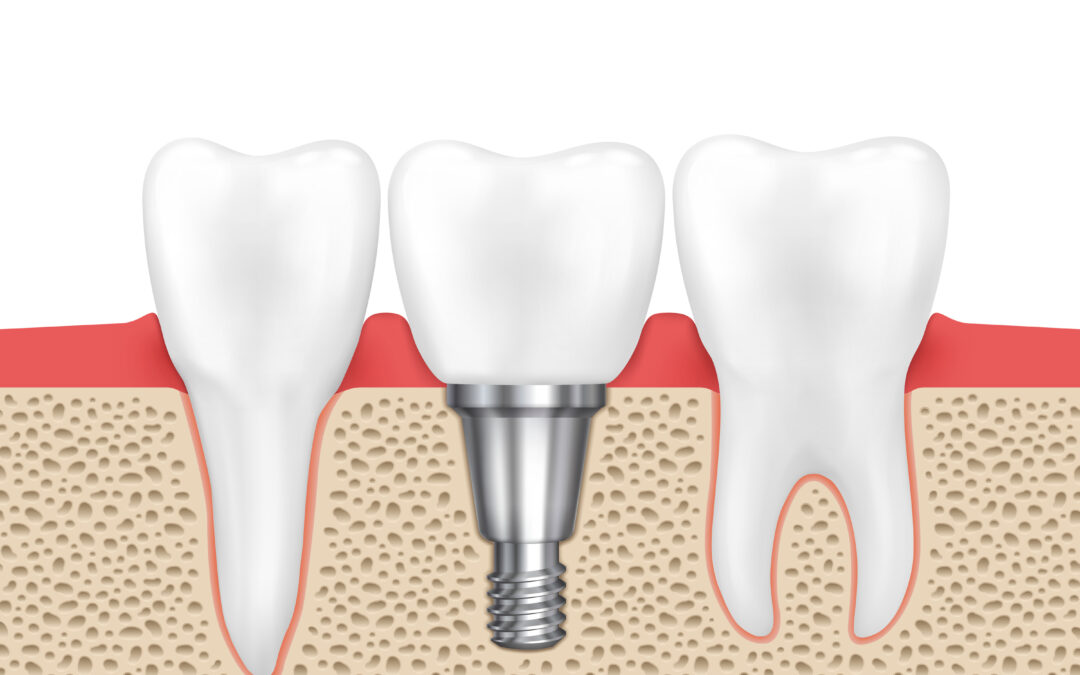
- Dental implants are unlikely to impact the rest of your mouth. When only one or a few teeth are failing, fixed bridges may be suggested as an alternative to an implant. However, unlike a bridge, dental implants do not require the adjacent natural teeth to be altered. Implants are impervious to tooth decay. They are also unlikely to cause gum disease if a patient follows a normal daily oral health care regimen.
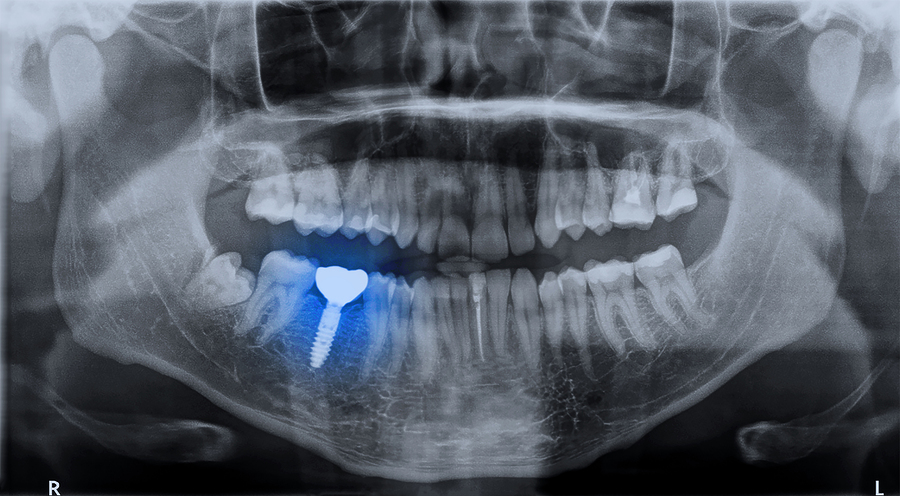
- Dental implants have proven to be safe for most adults who can undergo an extraction or other oral surgical procedures. Two key factors in determining if dental implant surgery is appropriate are gum health and the amount of bone density in the jaw. If a candidate for dental implants has healthy gums, has adequate bone density, and lacks any serious underlying systemic health condition, the implant procedure is usually considered safe.
- Dental implants, like root canals, have a very high long-term success rate. Longitudinal studies have shown that dental implants have a success rate of around 98 percent. What this means is that if you take care of your dental implant properly, it could last for decades, if not the rest of your life.
“When evaluating a patient to receive a dental implant, our practice considers many factors. When the circumstances are right, implants are a safe choice to replace missing or failing teeth,” says Dr. Jacqueline S. Allen, an endodontist practicing at the Phoenix Endodontic Group.

by Dr. Jacqueline S. Allen | Jun 25, 2019 | Blog, Dental Implants, Dentistry
As more people consider dental implants when natural teeth cannot be saved, some patients may wonder what level of discomfort to expect. This is a complex question, as some people need tooth extractions, sinus lifts, or bone grafts in conjunction with a dental implant. However, there are some general guidelines to how much pain is “normal” when you have a dental implant, and what kind of pain warrants a call to your dentist or endodontist.

When You Might Experience Pain During The Dental Implant Process
- During the implant procedure itself: This is possible, but not common, because your dentist will use the best type of anesthesia for your circumstances. This can include heavy local anesthesia and/or some type of sedation.
- After getting a dental implant: Once the anesthesia wears off, it is normal to experience swelling for the first three to four days after your operation and some pain may remain for as long as 7-10 days.
- If you had teeth extracted, a bone graft, or a sinus lift with your dental implant: All of these procedures can result in additional discomfort.
- If you experience complications during the healing process: If your post-op swelling goes away and then returns accompanied by pain, this may indicate you have an infection. Call your implant surgeon or endodontist – they may ask you return to be examined or may write you a prescription for an antibiotic.
Things You Can Do To Reduce Post-Operative Pain
- Take pain relievers as prescribed. Your dental implant provider will likely send you home with a prescription for ibuprofen or another pain reliever.
- Reduce swelling and pain with cold packs. Apply a cold pack or even a bag of frozen peas to the area of your cheek over the implant site. Avoid skin irritation by wrapping the cold pack in a thin cotton washcloth.
- Bathe the gums covering your implant with warm salt water. Do not swish! Hold the water in your mouth near the implant site, then spit it out gently. Repeat several times in a row, every few hours, for the first one to three days after your surgery.
“Dental implants can be a safe, durable, permanent solution for improving your oral health,” says Dr. Jacqueline S. Allen, an endodontist practicing at the Phoenix Endodontic Group. “Our staff can provide you with a comprehensive overview of how we can work together to minimize your pain during and after the implant surgery.”

by Dr. Jacqueline S. Allen | Mar 25, 2019 | Blog, Dental Implants, Phoenix Endodontic Group
When teeth are injured, infected, or structurally damaged, it can be challenging to determine the best path back to oral health. Sometimes endodontists can save natural teeth with root canals. When teeth are beyond saving, dental implants are an option. Implants are safe, remain securely in your mouth 24/7, and help prevent further jawbone loss. Properly cared for dental implants can last many years.

What The Research Says About Dental Implant Longevity
- Dental implants have been used reliably for more than 50 years. Implants are recognized as more effective than many types of bridgework.
- Root canal treatments and dental implants have similar levels of durability. Both restorations have a success rate of about 95 percent over post-implant periods as long as 16 years.
- Pre-implant oral health and post-implant oral care impact dental implant longevity. The best candidates for implants have healthy gums and enough jawbone density for support. Heavy smokers or patients with systemic conditions like diabetes must be evaluated for implants on a case-by-case basis. Following dental implant surgery, caring for the implant like a natural tooth is critical to ensuring its long-term endurance.
- Teeth grinding threatens dental implant success. The forces involved in grinding (bruxism) can damage the implant. Patients with bruxism who use a night guard or take other steps to control their teeth grinding can expect a better success rate.
“The choice to get dental implants should rest on the health of the teeth in question, the health of the patient, and their commitment to post-procedure upkeep,” says Dr. Jacqueline S. Allen, who practices with the Phoenix Endodontic Group. “Like root canals, the procedure has a high success rate under the right conditions.”
by Dr. Jacqueline S. Allen | Jan 23, 2019 | Blog, Dental Implants, Endodontist
When an injured or infected tooth cannot be saved, it’s natural to want to rush toward the next treatment step. If your choice to treat your failing tooth is a dental implant, your first question may be how long you have to wait after the extraction to get your dental implant. Just as every person’s mouth is unique, the timeline for their dental implant will be individualized. Several factors determine the length of time between extraction and implantation. 
What Can Impact Your Dental Implant Timeline?
- Number of teeth extracted. If one or two teeth are being extracted, it may be possible to proceed to an implant more quickly than if an entire arch of teeth are being removed.
- The health of your gums. If you have periodontal disease in addition to your compromised natural tooth, your dentist will want to improve the health of your gums before your implant.
- Whether you will need a bone graft to strengthen your jaw. If you have experienced bone loss in your jaw, you will likely need a bone graft to ensure the implant will be successful.
- The method of implantation your dentist has chosen. Extraction and implantation can be done the same day, but this requires a great deal of pre-planning and coordination between your dental professionals, as well specific criteria for your oral health. If a bone graft is needed, the implantation may need to allow for a healing period.
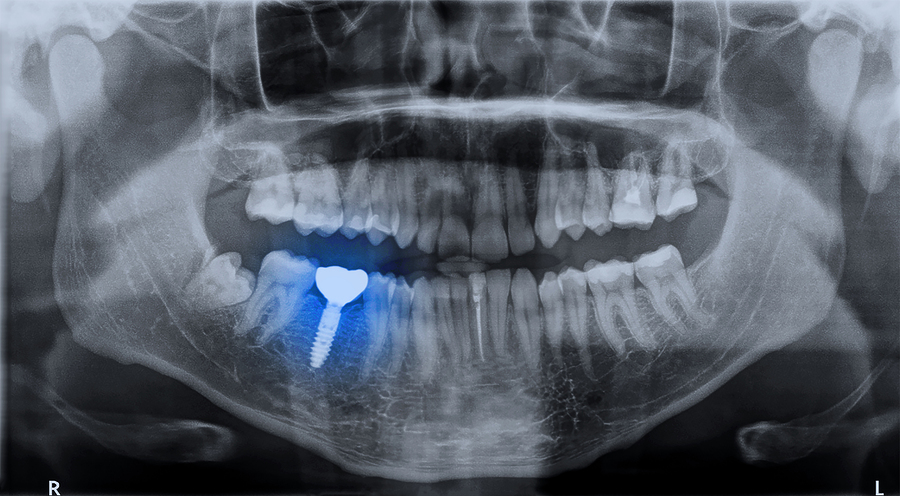
- How quickly the implant bonds to your jaw bone. Once your jaw is strong enough to accept a dental implant, the implant post will be placed. The process of osseointegration (the bone integrating with the implant) is what secures the implant and allows your new tooth to have a solid foundation.
“Dental implants have a high success rate, but only if the treatment is delivered in a way that meets the individual’s oral health needs,” says Dr. Jacqueline S. Allen, who practices with the Phoenix Endodontic Group. “If you have questions about how your procedure will unfold, ask your provider for a comprehensive explanation.”

by Dr. Jacqueline S. Allen | Nov 28, 2018 | Blog, Dental Implants, Dentistry, Endodontist, Phoenix Endodontic Group
 Dental patients with teeth that are seriously compromised by illness, injury, or decay are usually aware that extraction by itself is rarely the best option. If you are experiencing serious tooth trouble, you may be wondering whether a root canal or a dental implant would be the better solution.
Dental patients with teeth that are seriously compromised by illness, injury, or decay are usually aware that extraction by itself is rarely the best option. If you are experiencing serious tooth trouble, you may be wondering whether a root canal or a dental implant would be the better solution.
At Phoenix Endodontic Group, our practice is dedicated to saving natural teeth through root canal treatments and related procedures. However, there are times when a tooth simply cannot be saved through endodontic treatment. When that is the case, our practice may recommend a dental implant for the patient.
Who Is A Good Candidate For A Dental Implant?
- A patient who has a lower level of dental anxiety or phobia. Tooth extraction and implant surgery are more complex procedures than root canal treatment. If anxiety issues do exist, they should be discussed during preparation for the implant. We can develop a care plan for patients experiencing dental anxiety.
- A patient with strong periodontal (gum) health. By the time the “root canal or dental implant” crossroads has been reached, many patients already are struggling with advanced gum disease, but the healthier the gums are, the greater the likelihood the procedure will go smoothly.
- A patient who has not experienced significant bone loss in the jaw. Bone grafts can be done to strengthen a jaw before it receives an implant, but this may result in an additional procedure.
- A patient who can commit to a lengthy implantation/recovery process. Traditional dental implants require several months to complete. The portion of the implant inserted into the jaw must be allowed to integrate with the bone before placement of an artificial tooth is possible.
“Dental implants and root canals both have high levels of success and patient satisfaction,” says Dr. Jacqueline S. Allen, an endodontist who practices with the Phoenix Endodontic Group. “Your dental team can determine which treatment route is better for your individual circumstances.”
by Dr. Jacqueline S. Allen | Oct 24, 2016 | Blog, Dental Implants, Endodontics, Root Canal
 Dental implants have been offered in recent years as a panacea for fixing the problem of ailing teeth. However, the reality when it comes to treating a badly injured or infected tooth is more complex. Both endodontic procedures such as root canals and dental implants have their proper place – your dental care team can help determine what treatment will be most effective for you.
Dental implants have been offered in recent years as a panacea for fixing the problem of ailing teeth. However, the reality when it comes to treating a badly injured or infected tooth is more complex. Both endodontic procedures such as root canals and dental implants have their proper place – your dental care team can help determine what treatment will be most effective for you.
Here are four common myths related to dental implants, and the factual situation in each case.
Myths related to dental implants and root canal treatments
Myth #1: The best thing to do in all cases with an injured or infected tooth is to replace it with a dental implant.
There are a range of factors that will determine if a dental implant or a root canal is the best way to proceed. Although dental implants would appear at first glance to permanently resolve the issue with a troubled tooth, they can also cost more and require more visits to the dentist to complete. Most root canal treatments, which remove inflamed pulp and clean, fill and seal the inside of the tooth, can be accomplished in a single visit and are virtually painless.
Myth #2: Dental implants have a higher success rate than root canals.
A number of studies have shown both dental implants and root canals can have success rates of more than 95 percent. Currently, both procedures are considered excellent choices for treating an ailing tooth, and decisions to go with one procedure over the other should be based on factors related to an individual’s unique situation.
Myth #3: If you have a root canal and it fails, you need to have an extraction done and a dental implant placed.
Not necessarily. Root canals can fail for reasons that include damage to the crown protecting the treated tooth, additional tooth decay, or hidden canals that were not properly cleaned and filled the first time. However, endodontic retreatments of root canals can successfully restore the natural tooth to health in as many as 75% – 88% of all cases.
Myth #4: Your endodontist can’t help you if you need an implant.
Actually, the American Association of Endodontists has released a position statement affirming that if a endodontist determines a tooth must be extracted and a dental implant placed, he or she may proceed with the extraction and the placement of the implant if it is in the best interest of the patient.
“The decision whether to save a natural tooth or to proceed with an extraction and dental implant can be a difficult one,” says Dr. Jacqueline S. Allen, who practices with the Phoenix Endodontic Group. “Your endodontist can help you sort through your options and make the best decision for your individual health needs.”








 Dental implants have been offered in recent years as a panacea for fixing the problem of ailing teeth. However, the reality when it comes to treating a badly injured or infected tooth is more complex. Both endodontic procedures such as root canals and dental implants have their proper place – your dental care team can help determine what treatment will be most effective for you.
Dental implants have been offered in recent years as a panacea for fixing the problem of ailing teeth. However, the reality when it comes to treating a badly injured or infected tooth is more complex. Both endodontic procedures such as root canals and dental implants have their proper place – your dental care team can help determine what treatment will be most effective for you.