by Dr. Jacqueline S. Allen | Mar 15, 2016 | Blog, Endodontics, Root Canal
 Root canals have definitely evolved over the last several decades. For many years, root canals were synonymous with untoward events in people’s lives. Common phrases such as “I’d rather have a root canal than…” or “that hurt worse than a root canal” have haunted the specialty that I am so passionate about, for far too long. Even more recently, a comment made by our very own president painted root canals as being less popular than his bank buy-out. Come on people. Are root canals really that bad?
Root canals have definitely evolved over the last several decades. For many years, root canals were synonymous with untoward events in people’s lives. Common phrases such as “I’d rather have a root canal than…” or “that hurt worse than a root canal” have haunted the specialty that I am so passionate about, for far too long. Even more recently, a comment made by our very own president painted root canals as being less popular than his bank buy-out. Come on people. Are root canals really that bad?
The answer is simply, no; they are not! I have a phrase that I use when I complete a procedure and my patient says “well, that wasn’t as bad as everyone said it would be.” My reply is, “who wants to hear anyone say ‘my root canal was so easy; I didn’t feel a thing and it was a great experience?” Let’s face it, our world is so caught up in the horror stories that they believe to be true that they don’t really care or listen about the good experiences.
There have been so many advancements in root canal treatment! With the advent of new anesthetic techniques came the ability to treat teeth in one visit and with much less discomfort than before. With the advent of nickel titanium rotary, instruments are more efficient and have reduced clinical treatment times. With the advent of microscopes came the ability to see microfractures and additional canals that we never knew were there before. And with the advent of cone beam computed tomography, we gained the ability to discern between the teeth we should be treating, and those that are hopeless and should be extracted.
On March 27-April 2, the American Association of Endodontists will present its tenth annual Root Canal Awareness Week. This is a special week that we use to educate patients and remind clinicians of all the ways that root canal therapy has changed over the years. For the better!
Have a question about root canals? Leave a comment below or visit our website.

by Dr. Jacqueline S. Allen | Mar 8, 2016 | Blog, Endodontics, Endodontist, Root Canal
 No matter how permanent something seems in our lives, the element of change is always in play. Telephones have evolved from a device affixed to a wall that had us shouting into a large funnel to send our voice across the wires, into today’s “smartphones” that are basically tiny computers that fit in our pockets. We’ve transformed exercise gyms from places with vibrating motor-driven belts that jiggled our waists and thighs to slick suites offering Bikram “hot” yoga and Pilates.
No matter how permanent something seems in our lives, the element of change is always in play. Telephones have evolved from a device affixed to a wall that had us shouting into a large funnel to send our voice across the wires, into today’s “smartphones” that are basically tiny computers that fit in our pockets. We’ve transformed exercise gyms from places with vibrating motor-driven belts that jiggled our waists and thighs to slick suites offering Bikram “hot” yoga and Pilates.
Root canals – one of the key procedures used by endodontists to save weakened or infected natural teeth – have also evolved. The American Association of Endodontists showcase this progression during Root Canal Awareness Week, which this year will be observed from March 27 to April 2. The week casts a spotlight on how the root canal procedure has changed over the years and why endodontists are the best equipped providers to perform it.
Facts About Root Canals and Endodontists
- More than 15 million root canals are performed each year in the United States.
- Eighty-nine percent of patients who receive root canals from endodontists say that they are satisfied with the results they received.
- As root canal specialists, endodontists receive two to three extra years of training beyond dental school, and typically perform 25 root canals per week, compared to an average of less than two root canals performed each week by general dentists.
- Endodontists have the following advantages when they perform a root canal procedure: access to advanced equipment, knowledge of microsurgical techniques, and a professional focus on saving natural teeth and diagnosing and treating tooth pain.
“Family physicians turn to medical specialists, such as cardiologists and podiatrists, when their patients have serious health issues,” says Dr. Allen, an endodontist who practices with the Phoenix Endodontic Group. “General dentists turn to endodontists when your natural tooth needs to be treated with a root canal.”

by Dr. Jacqueline S. Allen | Feb 10, 2016 | Blog, Endodontics, Endodontist, Root Canal
 Having a root canal treatment is one big step toward saving an infected or damaged tooth. However, the root canal procedure itself, which has a 95 percent success rate, is only the beginning of the treatment process. There are several steps you can take – some immediately after your root canal and some over the long run – to ensure your tooth heals properly.
Having a root canal treatment is one big step toward saving an infected or damaged tooth. However, the root canal procedure itself, which has a 95 percent success rate, is only the beginning of the treatment process. There are several steps you can take – some immediately after your root canal and some over the long run – to ensure your tooth heals properly.
Caring For Your Teeth After A Root Canal
- Post-operative care. Immediately after the treatment, don’t bite down or chew with the treated tooth. You can manage discomfort with over-the-counter pain medication and by applying an ice pack to your face for 10 minutes every 20 minutes to reduce swelling. Return to your endodontist if discomfort persists or your original symptoms return.
- Taking prescribed medications. It is critical that you take all medications that may have been prescribed by your endodontist after your treatment.
- Dental restoration. Make an appointment with your general dentist around two weeks after your root canal so he or she can place a crown on the treated tooth to protect it from reinfection. A crown can also provide important support to the compromised tooth’s structure.
- Periodic endodontic appointments. Don’t skip follow-up visits to your endodontist after your restoration is in place. Your endodontist will examine the root canal by using X-rays and other assessment tools to make sure there are no signs of infection and to monitor healing.
- Good oral hygiene. You can keep your restored tooth healthy by brushing your teeth twice a day, flossing daily, and getting dental cleanings regularly.
“Some patients think their root canal is finished once they leave their endodontist’s chair,” says Dr. Allen, who practices with the Phoenix Endodontic Group. “But the treatment is a process, not an event. Following your aftercare instructions is crucial.”

by Dr. Jacqueline S. Allen | Jan 21, 2016 | Blog, Endodontics, Root Canal
 Tooth pain can be exasperating. Its intensity can range from barely perceptible to agonizing, but it’s difficult for the layperson to know exactly what’s wrong. One thing that anyone experiencing tooth pain should NOT do is ignore it. Here are four common causes of tooth pain, all of which can often require a root canal to address and treat the source of the pain properly.
Tooth pain can be exasperating. Its intensity can range from barely perceptible to agonizing, but it’s difficult for the layperson to know exactly what’s wrong. One thing that anyone experiencing tooth pain should NOT do is ignore it. Here are four common causes of tooth pain, all of which can often require a root canal to address and treat the source of the pain properly.
4 Causes of Tooth Pain That Can’t Be Ignored
- Cavities – Tooth decay can cause holes in our teeth, which can make them sensitive and cause pain. Small cavities can be rectified with fillings, but if left untreated, they can cause serious infections that impact the roots of your teeth and require a root canal to fix.
- Chipped or cracked teeth – Even a tiny bit of damage to your tooth enamel can become a gateway for bacterial infection in your teeth. If the chip or crack leaves a jagged or sharp surface, the tooth can cause pain by lacerating your gums or tongue.
- Bruxism – Bruxism, or grinding one’s teeth, can cause serious pain from the act of clenching one’s jaw. The condition can also lead to cracked teeth, which can also let infection enter the tooth.
- Dental injuries – Any kind of violent impact to the face or mouth can cause pain and damage to the entire tooth, including its root.
Symptoms that may indicate a condition that may require a root canal to address them can include pain when pressure is applied to a tooth, pain that appears with hot or cold foods/drink and remains after the hot/cold stimulus is removed, a pimple-like bump on the gums, or a swelling of the gums near a tooth.
“Pain is our body’s early warning system, telling us something is wrong with our teeth,” says Dr. Jacqueline S. Allen, an endodontist who practices with the Phoenix Endodontic Group. “Root canals and other related treatments can provide prompt, lasting relief.”

by Dr. Jacqueline S. Allen | Dec 7, 2015 | Blog, Endodontics, Phoenix Endodontic Group, Root Canal
 When a full-blown toothache happens, it can seem almost impossible to ignore. But sometimes it can be unclear what is happening, or what to do next.
When a full-blown toothache happens, it can seem almost impossible to ignore. But sometimes it can be unclear what is happening, or what to do next.
An infection in your tooth root that has abscessed is a serious matter. Here are a few facts about abscessed teeth that can help you make the right decision for your health quickly and get the treatment, including a root canal, that you may need.
What happens when a tooth becomes abscessed
A tooth abscess happens when there is an infection in or around the root of the tooth. Infection can enter a tooth due to decay, a crack or a chip in the tooth, or when periodontal (gum) disease becomes advanced and the infection enters through a pocket (gap) between the tooth and the surrounding gums. When there is an abscess, the pulp inside of a tooth dies and may become inflamed.
Symptoms of a tooth abscess
Often patients with a tooth abscess will feel an ache in the bone around the tooth. This may start as a throbbing pain that won’t go away. Sensitivity in the tooth to heat and when chewing may also be present. Later, a fever may develop, or lymph nodes under the jaw or in the neck may swell and become tender. If the abscess breaks open, a sudden rush of foul-smelling and foul-tasting fluid (pus) may spill into the mouth.
After acute pain passes and the diseased pulpal tissue dies, the pain may fade, or even go away, but the problem won’t.
Treating an abscessed tooth
A dental specialist such as an endodontist should evaluate a tooth that may be abscessed. They will take a detailed history of the pain symptoms, test the responsiveness of the tooth to temperature and pressure, and evaluate radiographs (x-ray pictures) in order to help make a diagnosis.
It’s important to determine the origin of the infection. If the infection is inside the tooth’s pulp, a root canal treatment, with an appropriate restoration applied afterward, can ensure the infection doesn’t return. If it is a serious periodontal infection causing the abscess, the gums also will need to receive treatment to prevent the spread of the infection.
“Always take toothache symptoms seriously,” says Dr. Allen, an endodontist with the Phoenix Endodontic Group. “Get a professional evaluation. If it is being caused by an abscessed tooth, a root canal treatment can often save the tooth and keep it healthy for years to come.”
by Dr. Jacqueline S. Allen | Nov 30, 2015 | Blog, Endodontics, Root Canal
 Having a clear idea about what a root canal entails is the first step toward knowing whether it is the right treatment for your dental challenges. Dr. Jacqueline S. Allen of the Phoenix Endodontic Group says, “It’s important for patients to understand the root canal process. Having full comprehension of what’s really involved in this procedure can make it easier for them to make truly informed decisions about their oral health.”
Having a clear idea about what a root canal entails is the first step toward knowing whether it is the right treatment for your dental challenges. Dr. Jacqueline S. Allen of the Phoenix Endodontic Group says, “It’s important for patients to understand the root canal process. Having full comprehension of what’s really involved in this procedure can make it easier for them to make truly informed decisions about their oral health.”
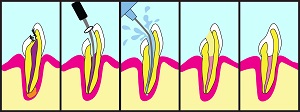
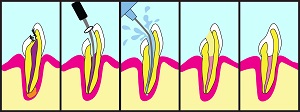
The Root Canal Process
- A patient presenting with symptoms of pain, tooth discoloration, prolonged sensitivity to heat or cold, or tenderness to the touch or when chewing is referred to an endodontist for diagnosis.
- The endodontist will examine the tooth and take X-rays to determine if the pulp of the tooth is infected and/or inflamed. If so, an appointment to perform a root canal treatment will be set up.
- On the day of the root canal treatment, the endodontist may numb the treatment area with a local anesthetic and place a dental dam around the affected tooth to keep it free of saliva and debris.
- Next, the dentist will access the root canals of the tooth through its crown, and use special metal files to clean the canals and remove the infected pulp from the tooth.
- After the pulp is removed, the endodontist will fill the canals with a bio-compatible material known as gutta-percha. A temporary filling will be placed in the tooth opening to seal off the canals.
- When the patient returns to the endodontist, the temporary filling will be removed, to make way for a crown or other permanent restoration to be placed by a restorative dentist. If the tooth lacks structure to hold the restoration in place, the endodontist or restorative dentist may place a post in the tooth.
Re-treatment of the tooth with the root canal may be needed later if it becomes injured or suffers additional tooth decay. In both cases, the sealed canals could be exposed to additional infection or inflammation.
“The root canal process is fairly straightforward, and has a success rate of about 90 percent,” Dr. Allen says. “Clarity about what to expect can help patients who need this procedure feel more confident that they are making an excellent choice for their health.”

 Root canals have definitely evolved over the last several decades. For many years, root canals were synonymous with untoward events in people’s lives. Common phrases such as “I’d rather have a root canal than…” or “that hurt worse than a root canal” have haunted the specialty that I am so passionate about, for far too long. Even more recently, a comment made by our very own president painted root canals as being less popular than his bank buy-out. Come on people. Are root canals really that bad?
Root canals have definitely evolved over the last several decades. For many years, root canals were synonymous with untoward events in people’s lives. Common phrases such as “I’d rather have a root canal than…” or “that hurt worse than a root canal” have haunted the specialty that I am so passionate about, for far too long. Even more recently, a comment made by our very own president painted root canals as being less popular than his bank buy-out. Come on people. Are root canals really that bad?

 No matter how permanent something seems in our lives, the element of change is always in play. Telephones have evolved from a device affixed to a wall that had us shouting into a large funnel to send our voice across the wires, into today’s “smartphones” that are basically tiny computers that fit in our pockets. We’ve transformed exercise gyms from places with vibrating motor-driven belts that jiggled our waists and thighs to slick suites offering Bikram “hot” yoga and Pilates.
No matter how permanent something seems in our lives, the element of change is always in play. Telephones have evolved from a device affixed to a wall that had us shouting into a large funnel to send our voice across the wires, into today’s “smartphones” that are basically tiny computers that fit in our pockets. We’ve transformed exercise gyms from places with vibrating motor-driven belts that jiggled our waists and thighs to slick suites offering Bikram “hot” yoga and Pilates.
 Having a root canal treatment is one big step toward saving an infected or damaged tooth. However, the root canal procedure itself, which has a 95 percent success rate, is only the beginning of the treatment process. There are several steps you can take – some immediately after your root canal and some over the long run – to ensure your tooth heals properly.
Having a root canal treatment is one big step toward saving an infected or damaged tooth. However, the root canal procedure itself, which has a 95 percent success rate, is only the beginning of the treatment process. There are several steps you can take – some immediately after your root canal and some over the long run – to ensure your tooth heals properly.
 Tooth pain can be exasperating. Its intensity can range from barely perceptible to agonizing, but it’s difficult for the layperson to know exactly what’s wrong. One thing that anyone experiencing tooth pain should NOT do is ignore it. Here are four common causes of tooth pain, all of which can often require a root canal to address and treat the source of the pain properly.
Tooth pain can be exasperating. Its intensity can range from barely perceptible to agonizing, but it’s difficult for the layperson to know exactly what’s wrong. One thing that anyone experiencing tooth pain should NOT do is ignore it. Here are four common causes of tooth pain, all of which can often require a root canal to address and treat the source of the pain properly.