by Dr. Jacqueline S. Allen | Jun 22, 2021 | Blog, Endodontics, Endodontist, Phoenix Endodontic Group, Root Canal
Although root canal treatments have an overall success rate that exceeds 90 percent, patients who have never needed endodontic treatment may be concerned with how much time it will take to recuperate. The good news is that most people can go back to work or school the day after a root canal treatment. However, it often requires two visits to complete a root canal, spaced out over several weeks’ time, depending on individual circumstances.
You can make your recovery after a root canal treatment as smooth as possible by following a few simple guidelines in the hours, days, and weeks after treatment.
 Root Canal Treatment Recovery Tips
Root Canal Treatment Recovery Tips
Hours after your procedure: It’s possible to experience discomfort after your root canal, but this is usually mild to moderate for most people and can be easily managed with over-the-counter pain relievers. You can protect your newly treated tooth by making sure that you:
- Eat soft foods, such as applesauce or yogurt, that require little chewing.
- Avoid hot or crunchy foods.
- Minimize chewing with the tooth that’s been treated.
Days after your procedure: If you had pain before your procedure, it’s possible you’ll have sensitivity in the tooth that received the root canal treatment. If over-the-counter pain relievers are not effective, you should contact your endodontist for further instructions. Also, while you should immediately resume brushing and flossing after your root canal, take extra special care with the area around the affected tooth so as not to dislodge the temporary filling that the endodontist placed over the root canal to keep it sanitary and protected.
Weeks after your procedure: Any discomfort you have in the days after your root canal should subside quickly. If the pain does not go away, or increases, call your endodontist for a recheck. Pain can be an indicator that the tooth has become re-infected, or has an undetected crack.
Also, you should make an appointment with your endodontist for some weeks after your initial root canal treatment to have a permanent restoration, usually a crown, placed over the top of the treated tooth. This is essential to keeping your natural tooth healthy for a lifetime.
“One of the most essential tools when recovering from a root canal treatment is open communication with your endodontist,” says Dr. Jacqueline S. Allen, who practices with the Phoenix Endodontic Group. “Your practitioner can help you understand how your recovery is progressing, and evaluate whether follow-up care is needed.”
by Dr. Jacqueline S. Allen | May 21, 2021 | Blog, Endodontist, Phoenix Endodontic Group, Root Canal
COVID-19 and its social and economic effects have made 2020 and the beginning of 2021 extraordinarily difficult in many ways. For some of us, it has moved the impact of our daily health routines to the front of our minds. For those with injured, damaged or infected teeth, understanding the urgency of receiving timely endodontic treatment can be of critical importance.
Each May, the American Association of Endodontists focuses on promoting the importance of saving natural teeth. This year’s theme is “Worth Saving!” and as you’ll soon see, there are plenty of reasons to consider root canals or other types of endodontic treatment your first choice for treating your dental problem.
Your Natural Teeth ARE Worth Saving – Here’s Why
- The consequences of losing your tooth or having it extracted can be serious. Your mouth is designed to operate with a full set of natural teeth. Remove one (or more), and the remaining teeth will shift, impacting both the appearance of your smile and your ability to chew.
- The cost of replacing your natural tooth with an artificial one can be substantial. Sometimes a dental implant is the best choice when your natural tooth simply is beyond repair. However, implants can be costly, and while the implant is healing, you may not be able to use that tooth as you normally would.
- Endodontists have extra training and specialized experience in saving teeth. Your general dentist likely has a close partnership with one or more endodontists, upon whom they can rely if one of your natural teeth is endangered. The entire focus of endodontic treatment is saving natural teeth. Endodontists receive two to three years of additional training after becoming a dentist, and once they are in practice, they may perform an average of 25 root canals per week (versus two per week for general dentists).
- Modern root canals and other endodontic treatments effectively relieve pain. Patient perceptions of root canals are changing; in the last generation, improvements in pain management and endodontic technique have greatly reduced postoperative discomfort for root canals. If you come into a root canal with a severely infected tooth, it’s likely the procedure will completely eliminate your pain after a brief recovery period.
“Our job as endodontists is to preserve your natural teeth,” says Dr. Jacqueline S. Allen, who practices with the Phoenix Endodontic Group. “From root canals to retreatments to apicoectomies and more, we have a broad range of options to bring your teeth back to full functioning.”
by Dr. Jacqueline S. Allen | Apr 22, 2021 | Blog, Endodontics, Endodontist, Phoenix Endodontic Group, Root Canal
For many years, comedians have regularly used the term “root canal” to capture any painful experience. The jokes weren’t funny to anyone who actually needed a root canal – fear of pain was sometimes enough to keep them from getting badly needed care.
Today’s root canals, though, have advanced dramatically in terms of technique and technology from 20 or even 10 years ago. In many cases, a root canal now relieves dental pain, instead of intensifying it.
Your endodontist is trained in pain management for root canals and other procedures that involve the roots and nerve pulp of your teeth. The amount of discomfort you experience during and after a root canal will vary with your individual circumstances, but here are some of the most common factors that can impact your pain level.
What Factors Influence Root Canal Pain?
- The amount of infection in or damage to the tooth prior to the procedure. Root canals are performed on teeth with infected, inflamed, or damaged tooth pulp. One common symptom of tooth pulp damage is persistent tooth pain. If your tooth is badly infected before your root canal, it can also be more sensitive afterward.
- How you use pain relievers after your root canal. Some tenderness and sensitivity is expected after the procedure. Your endodontist can provide guidance on when to take over-the-counter pain relievers and what kind of dosing schedule to maintain until the pain is no longer a distraction.
- How closely you listen to and follow post-procedure instructions from your endodontist. After your root canal, you will want to avoid chewing with the affected tooth until it has received a permanent dental restoration (typically a crown). You will also want to choose soft, cool foods like applesauce or yogurt to eat for the first few days. Hard, hot, or crunchy foods increase the likelihood you will feel sensitivity or pain when you eat.
- How quickly you report any severe post-procedure pain. It’s imperative you call your endodontist right away if you experience sharp or severe pain after your root canal; this can indicate that infection has returned. You will need to be seen to assess the situation, and your endodontist can plan additional pain and infection management steps.
“Today’s root canals rarely involve severe pain,” says Dr. Allen, who practices at the Phoenix Endodontic Group. “Your endodontist is your partner in managing discomfort after a root canal and is the first person you should call if that pain becomes severe.”

by Dr. Jacqueline S. Allen | Feb 22, 2021 | Blog, Endodontics, Endodontist, Phoenix Endodontic Group, Root Canal
While more and more Americans are becoming aware of the benefits of preserving natural teeth, you may still find yourself with a number of questions and no little anxiety when a root canal is the suggested option for saving a diseased or damaged tooth. Root canals can be an intricate procedure, depending on the extent of the damage to the tooth. Occasionally, sedation is called for. However, most of the time, patients are awake during the procedure and fully aware of each step the endodontist is taking. Each case is different, though, so let’s look at the issue a little more broadly.

How Endodontists Manage Pain And Patient Awareness During Root Canals
- For most root canals, local anesthesia is used to numb the area around the affected tooth. This is a necessary step because your endodontist will be removing pulp and nerve fibers from your tooth. You will likely be fully awake during the entire procedure. Your mouth, including your lips, may feel numb for several hours after the procedure, so it is important to be careful if you eat or drink before full feeling returns to the numbed area. Be sure to follow your endodontist’s guidelines for eating and drinking, though.
- For patients with dental anxiety or dental phobia, some level of sedation may be necessary for the root canal to be a success. Sedation can range from minimal (just to take the edge off your jitters) to deep (where you may be barely conscious, but able to be awakened). It can be delivered by inhalation, orally, or intravenously. General anesthesia – during which you are completely unconscious – is rarely used for root canals and requires special training to safely administer.
Dr. Allen, of the Phoenix Endodontic Group, encourages patients to discuss questions related to wakefulness and anxiety with their endodontist during the planning stages of their root canal. “In our practice, we make sure all our patients are fully informed and arrive ready for their root canal,” she says. “We can discuss your individual needs prior to beginning the procedure and offer solutions that will help you feel comfortable, safe, and pain-free.”
by Dr. Jacqueline S. Allen | Dec 21, 2020 | Blog, Endodontics, Endodontist, Root Canal
It’s crucial to have accurate information when considering a root canal. A qualified general dentist or endodontist can offer up-to-date knowledge about how root canals work and why you might need one.
Here are five common root canal questions received at the Phoenix Endodontic Group.
5 Top Root Canal Questions – Answered.
- What symptoms indicate a root canal may be needed? Natural teeth that are candidates for root canals have typically been damaged by decay or infection, or suffered structural damage to the tooth. Symptoms that may call for a root canal include: a severe toothache when you chew or apply pressure to the affected tooth; prolonged sensitivity to hot or cold; a recurring pimple on the gums near the tooth; discoloration of the tooth; swelling or tenderness in adjacent gum tissue.
- Will a root canal hurt? Today’s root canal procedures typically relieve pain created by infection or damage to the nerves inside the tooth pulp, rather than causing pain. Additionally, endodontists receive special training in pain management, so even post-operative discomfort is typically minimal.
- Is a root canal a better option than having my tooth pulled? The answer to this question depends on the overall health of your tooth, the gums surrounding it, and whether other natural teeth are suffering advanced decay or infection. One noteworthy advantage to retaining your natural teeth is a reduced chance of bone loss in your jaw. Such loss can lead to a host of negative consequences.
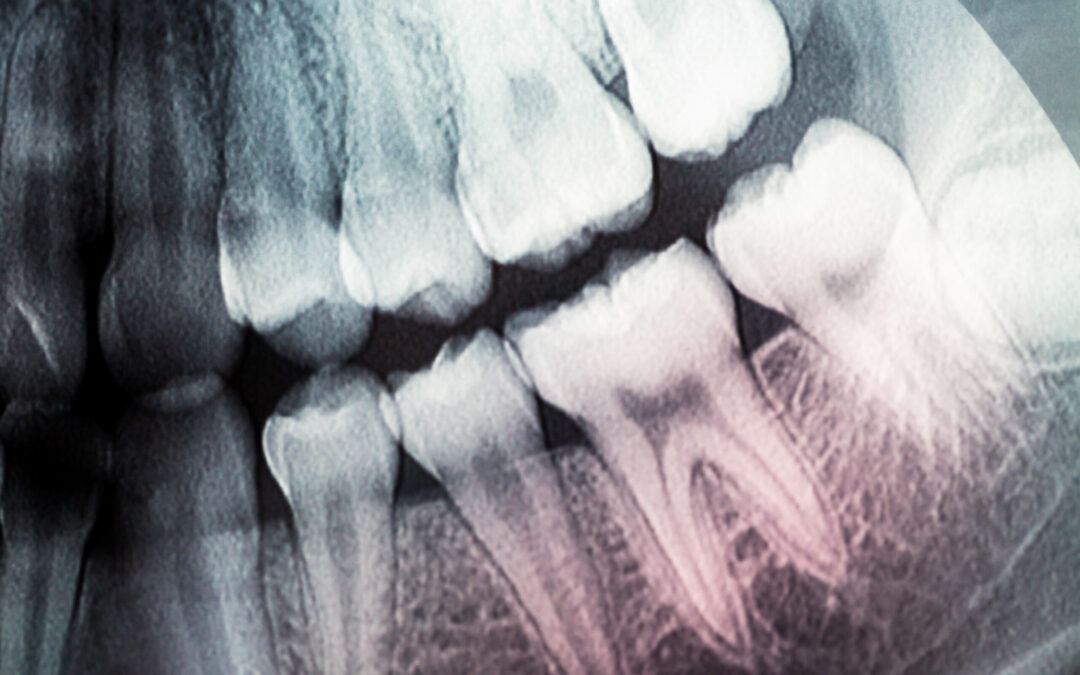
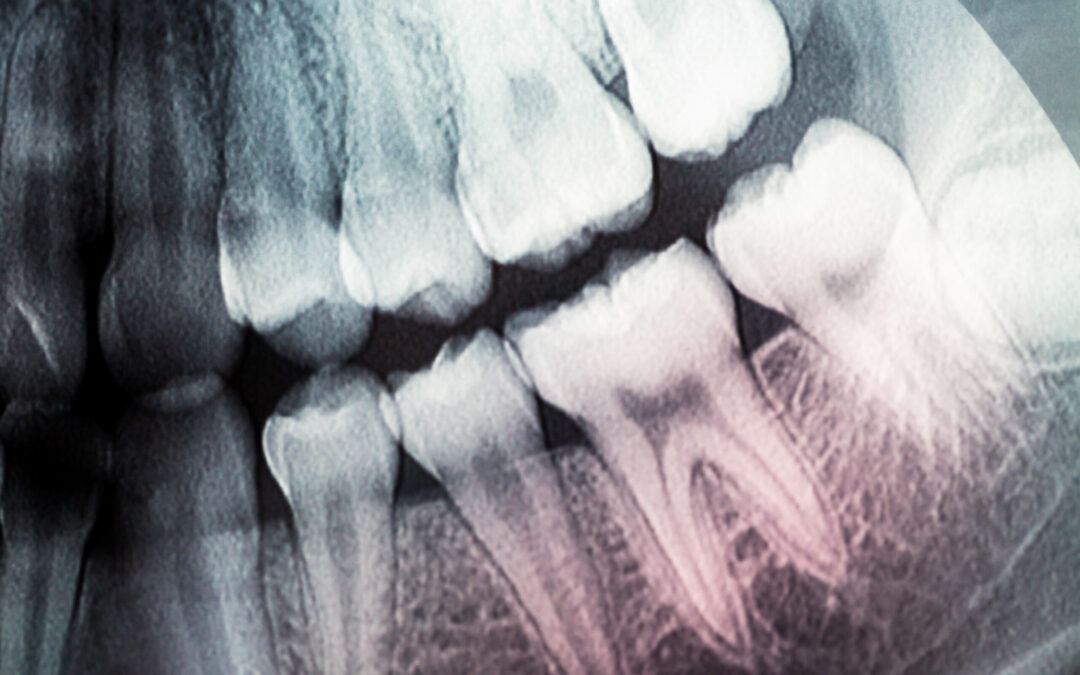
- What happens during a root canal? Here is a brief overview of how a root canal is performed: First, your endodontist will take X-rays. Then, they will numb the area with a local anesthetic and place a dental dam over the tooth to protect it from bacteria. Next, the practitioner will drill an access hole in the crown of the tooth. The pulp chamber and roots of the tooth will be thoroughly cleaned, shaped with special tools, then filled with a biocompatible material. Once complete, the endodontist covers the opening with a temporary filling. Weeks later, the final step in the procedure takes place: placing a crown, permanently sealing the access hole.
- Does it take a long time to recover after a root canal? Most patients experience some mild tenderness in the area of the root canal for a few days. This is usually managed with over-the-counter or prescription pain relievers. This discomfort should disappear within a week. If you experience severe pain, significant swelling, or if your temporary filling falls out, contact your endodontist as soon as possible so they can examine the tooth.
“It’s normal to be apprehensive if you have never had a root canal before,” says Dr. Allen, who practices with the Phoenix Endodontic Group. “Our office is always happy to answer your questions about root canals and provide you with a more comprehensive view of the procedure.”
by Dr. Jacqueline S. Allen | Oct 12, 2020 | Blog, Endodontics, Phoenix Endodontic Group, Root Canal
Many dental patients know that root canals can save natural teeth but may wonder what actually happens inside the tooth with the procedure. Of course, there are many benefits to retaining your natural teeth whenever possible. The root canal treatment procedure replaces the living nerve pulp of your tooth with an inert biocompatible material, usually gutta-percha. Here’s a quick look at how root canals impact your natural tooth and allow them to remain a part of your smile.

How A Root Canal Affects Your Tooth
- The root or nerve pulp. This is the part of a tooth’s anatomy most impacted by a root canal. Typically, a root canal is called for if the tooth nerve has died or if the pulp is badly infected. During a root canal, the nerve pulp is removed with special tools and the canals themselves are flushed with material to treat the infection, so it does not return.
- The dentin. This layer of calcified tissue supports the top layer of enamel in a natural tooth. Dentin is produced by nerve pulp, so once the pulp is replaced with gutta-percha, dentin will no longer be produced in that tooth, which may make your teeth more brittle.
- The enamel. This hard outer layer of your natural tooth protects the internal parts of your tooth. It can be compromised by tooth decay or dental injuries (cracked or broken teeth), allowing bacteria to invade your nerve pulp chamber. A root canal stops this process, because not only does it remove the infected nerve pulp, the finishing restoration – a crown – fits like a “cap” over the tooth enamel, protecting it from additional damage or bacterial intrusion.
- The periodontal ligament. Sometimes a tooth is damaged because it is pushed out of position, threatening the periodontal ligament, which attaches our natural tooth to the jaw. In this case, a root canal can prevent further damage to the tooth, allowing it to be splinted in place to encourage the periodontal ligament to reattach and preventing infection issues inside the tooth.
While root canals do not “kill” natural teeth, removing and replacing the nerve pulp makes the tooth more brittle. Your endodontist will determine if you need additional restorations beyond a crown to ensure your tooth has sufficient support to function normally.
“Root canals do change how your natural teeth function, but they allow the other structures that are part of your teeth and gums to return to health, supporting your overall oral wellbeing,” says Dr. Allen, who practices with the Phoenix Endodontic Group. “Our practice is always happy to explain precisely how endodontic treatment can help preserve your natural teeth.”

 Root Canal Treatment Recovery Tips
Root Canal Treatment Recovery Tips