by Kevin Conroy | Apr 8, 2024 | Phoenix Endodontic Group
Ever since May of 2023 when Dr. James Wolcott started working at Phoenix Endodontic Group, he is always towing his “toy hauler” and leaves it in the parking lot while he is treating patients during work hours. After work, he would always say “Oliver and I are going to race karts at the track tonight.” (Oliver Wolcott is Dr. Wolcott’s (almost) 15-year-old son. Oliver is a Freshman at Brophy College Prep). This weekend, Dr. Allen and I decided to see what “the track” was all about.
Little did we know that off the Pinnacle Peak exit from the I-17 in North Phoenix/ Glendale are parcels of land that house a water park, railroad museum and Phoenix Kart Racing Association (PKRA) and their kart racing track. Dr. Wolcott arranged for us to get pit passes for the day – we showed up to get a view of the action and cheer on our friends.
When we got there, we saw Dr. Wolcott pushing (on a gurney) Oliver’s kart back to his make shift shop (the toy hauler) for some repairs. On Oliver’s practice run, his chain came off and forced him onto the infield. In this league, you need to be prepared and Team Wolcott sure was. The tires came right off so Dr Wolcott could get to the chain to do the repairs necessary to have the kart ready for the qualifying heats later in the morning.
In total there were 9 categories of racers, starting with kids as young as 5 years old. The categories go up to the Master Class – adults that enjoy the sport. We watched the first 8 races in anticipation of seeing Oliver & Dr Wolcott race in the 9th heat. What a thrill it was for Dr. Allen and I to watch a race with two of our “team” participating. Afterwards, Dr. Wolcott told me that Oliver’s kart got up to 71mph!
This was such a fun activity for us on a beautiful Sunday morning in Phoenix. Surely, we will be back, hopefully with more of the team from Phoenix Endodontics to cheer on our friends and colleague – Dr. Wolcott & Oliver. Great work today guys!
So, if you are ever visiting the Phoenix Endodontic Group office and you see a white toy hauler trailer in the parking lot – you know Dr James Wolcott is close by.
Watch this short video of racing at PKRA.

by Dr. Jacqueline S. Allen | Mar 21, 2023 | Blog, Endodontics, Endodontist, Phoenix Endodontic Group, Root Canal
Pain sends many patients to the dentist. This is certainly the case when it comes to patients who need root canals. However, not feeling pain does not mean you don’t need a root canal.
Root canals are an endodontic technique to preserve natural teeth that have irreversible pulpitis, an infection of the nerve pulp of a tooth not able to be treated successfully. This condition can result from severe decay or an injury to the tooth. Often there is pain, but not always.
Here are a few important reasons to look beyond pain to discover whether your tooth needs a root canal treatment.

Looking Beyond Pain – Root Canal Treatment
-
Your endodontist is looking for infection as the cause of your troubles, not pain. Inflammation in the tooth’s nerve pulp is the cause the endodontist is looking for. Pain can accompany inflammation, but it is not a reliable guide to diagnosis.
-
Pain is only one symptom of needing a root canal. Other symptoms include teeth that are sensitive to heat or cold, swelling of the face or gums, or teeth that become gray or discolored.
-
Your infection may be draining, perhaps temporarily reducing pain, but also pouring foul toxins into your mouth. A pimple on the gum, called a fistula, or other types of pus drainage from the tooth are also symptoms of pulpitis. These conditions may temporarily reduce your pain, but the tooth will still need treatment: a root canal.
-
Pain associated with inflamed nerve pulp can be inconsistent. If your dentist puts you on an antibiotic to deal with an infected tooth, your pain may be relieved. Your pain may go away on its own, but this might be because the nerves in your tooth have died – not because the tooth is healthy again. Some patients who require root canals report “positional pain,” pain that emerges only when they sit up, lay down, or run in place.
“Determining whether a patient needs a root canal can be complex, and pain is only one factor considered in an evaluation,” says Dr. Jacqueline S. Allen, who practices with the Phoenix Endodontic Group. “Regular checkups with your general dentist and referrals to endodontic specialists as needed are the most reliable way to know if your natural teeth need a root canal to save them.”

by Dr. Jacqueline S. Allen | Nov 21, 2022 | Blog, Endodontics, Endodontist, Phoenix Endodontic Group, Root Canal
It can be a shock to learn you require root canal therapy to address an injured or infected tooth. If you’ve never been to an endodontist, or don’t have any friends or family who’ve had a root canal, you may naturally have a lot of questions about what to expect.
Understanding the details of root canal therapy can help you come to your first appointment better prepared. Here is a brief overview of the main stages of a root canal.
 The Key Stages Of Root Canal Therapy
The Key Stages Of Root Canal Therapy
-
Confirmation of diagnosis. Your endodontist will confirm your diagnosis when you arrive for your first root canal therapy appointment by reviewing your X-rays and performing a visual inspection of your tooth.
-
Local anesthesia and dental dam placement. The endodontist will numb the area around your tooth with a local anesthetic. They will also place a rubber sheet known as a dental dam around the tooth to keep it clean and dry while they work.
-
Creating an access hole. After the tooth has been prepared and your gums numbed, an access hole will be drilled in the crown of the tooth to allow the dental pulp to be removed.
-
Pulp removal, filing, and cleaning. Once the access hole is created, the endodontist removes the infected tooth pulp, using special instruments to reshape the tooth’s canals and ensure all infected material is gone. Then the inner tooth is treated with antimicrobial washes to remove debris and aid healing.
-
Filling the root canals. This is the step that gives root canal therapy its name. A biocompatible material, usually gutta-percha, is used to fill the canals and prevent future infections.
-
Placement of temporary filling. The first part of the root canal procedure concludes with a temporary filling on your tooth to ensure the tooth heals and bacteria is not re-introduced while your permanent restoration is being fabricated.
-
Placement of permanent filling and crown. Your root canal therapy is not considered complete until a permanent filling is placed on your tooth, AND the tooth is capped with a crown. A crown provides extra protection against infection and shores up the structural integrity of your natural tooth.
“Patients are surprised sometimes to find out that root canal therapy follows a simple, straightforward process,” says Dr. Jacqueline S. Allen, who practices at Phoenix Endodontic Group. “But our profession’s approach to this procedure has been developed and refined for more than 150 years. We’re happy to explain each step in detail, and to address any concerns or questions you may have, every step of the way. We want each of our patients to be comfortable and confident.”

by Dr. Jacqueline S. Allen | Sep 21, 2022 | Blog, Dental Implants, Dentistry, Phoenix Endodontic Group
If you have a failing tooth (or teeth), you may be wondering if a dental implant might be a workable solution for you. Implants take the place of your natural teeth. They are anchored to your jawbone, and topped with an artificial tooth. Dental implants have a similar success rate to root canals, when performed by a dentist or endodontist with significant experience doing them. They are not, however, the ideal solution for every patient.
Let’s take a look at some factors to consider before getting a dental implant.

What Important Factors Should I Consider Before Getting A Dental Implant?
-
Are there less invasive options that could save the tooth? In some cases, a tooth that is threatened by infection, decay, or advanced gum disease may be able to be saved. Root canal treatment and periodontal (gum) procedures may be solid alternatives; your dental provider will be able to discuss their potential to help you.
-
Have I discussed my health conditions with my provider? The endodontist or implantologist who performs your dental implant will conduct a thorough examination, and take images of your teeth. They will also ask about your medical history. You should discuss any serious conditions such as diabetes or cardiovascular disease. You should also let your provider know if you’re a heavy smoker or if you’ve had radiation therapy to your head or neck.
-
Will I need additional procedures to prepare for my dental implant? Depending on your individual circumstances, you may need a sinus lift, tooth extraction or removal of parts of your damaged tooth, bone augmentation, gum treatment, or other procedures to prepare for your dental implant. Your provider can explain the need for each procedure and how it fits in your treatment timeline.
-
Will I have to commit to multiple appointments over a number of months to complete the dental implant process? Depending on the approach that your provider recommends, you may need to come to a number of appointments to plan, prepare for, and undergo all the procedures that complete your dental implant. Discuss any scheduling constraints with your dental professional and their staff.
“To ensure that a dental implant is the right approach to improve your oral health, our staff will discuss all relevant factors impacting the process before treatment begins,” says Dr. Jacqueline S. Allen, who practices with the Phoenix Endodontic Group. “This ensures your treatment team has all the information needed to provide excellent treatment. It also gives peace of mind that you are making the right choice.”

by Dr. Jacqueline S. Allen | Aug 19, 2022 | Blog, Endodontics, Endodontist, Phoenix Endodontic Group, Root Canal
Patients often ask our staff at Phoenix Endodontic Group questions about their root canals looking to better understand what they will experience. Many people are concerned about the severity of the procedure or how much recovery time to plan for.
The good news is that many root canals have a quick recovery time – often just a week of special post-operative care. Many factors can impact your individual outcome, though, so it is important to understand the circumstances that brought you to the endodontist in the first place. Here’s a short list of some situations that can make the root canal procedure itself or your post-op period require extra care to ensure the root canal is successful.
 What Makes A Root Canal A Serious Procedure?
What Makes A Root Canal A Serious Procedure?
-
When there is pre-existing infection or tooth damage. A crack or chip can let infection deep into a tooth’s pulp. Extensive tooth decay can also reach the pulp. If the infection causes an abscess, antibiotics may be needed first to eliminate the bacteria so the root canal can safely seal the roots so infection does not happen again.
-
When the tooth involved has multiple roots. The level of complexity involved with cleaning and sealing canals during a root canal increases with the number of canals in the tooth receiving treatment. Molars have up to four canals; premolars have one or two; canines and incisors have just a single canal.
-
When you don’t contact your endodontist if you have aftercare problems. An ordinary root canal can escalate quickly to challenging if you do not promptly call your endodontist when you experience pain that is severe or rapidly increasing; if the temporary filling placed in the tooth comes out; or if you can see swelling inside or outside of your mouth.
-
When you don’t return for your permanent crown as scheduled. The tooth being treated with a root canal should receive a permanent crown about two weeks after the procedure. Crowns provide structural support, protect the tooth from infection, and reduce nerve sensitivity to hot or cold foods and beverages. Not getting a permanent crown leaves your tooth vulnerable to further damage or infection and possible the failure of the root canal.
“The seriousness of each root canal is impacted by a patient’s individual oral health,” says Dr. Allen, of the Phoenix Endodontic Group. “We are happy to explain our assessment of your situation and provide tips for making your root canal successful and stress-free, so it can help you hold on to your natural tooth for the rest of your life.”
by Dr. Jacqueline S. Allen | Jul 20, 2022 | Blog, Endodontics, Endodontist, Phoenix Endodontic Group, Root Canal
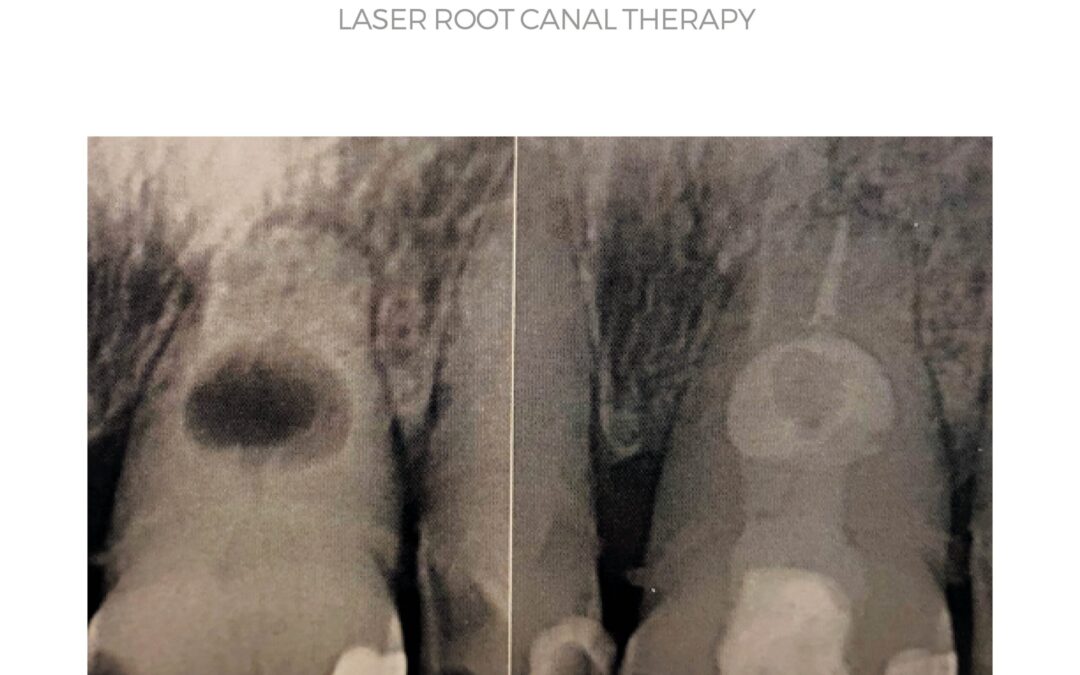
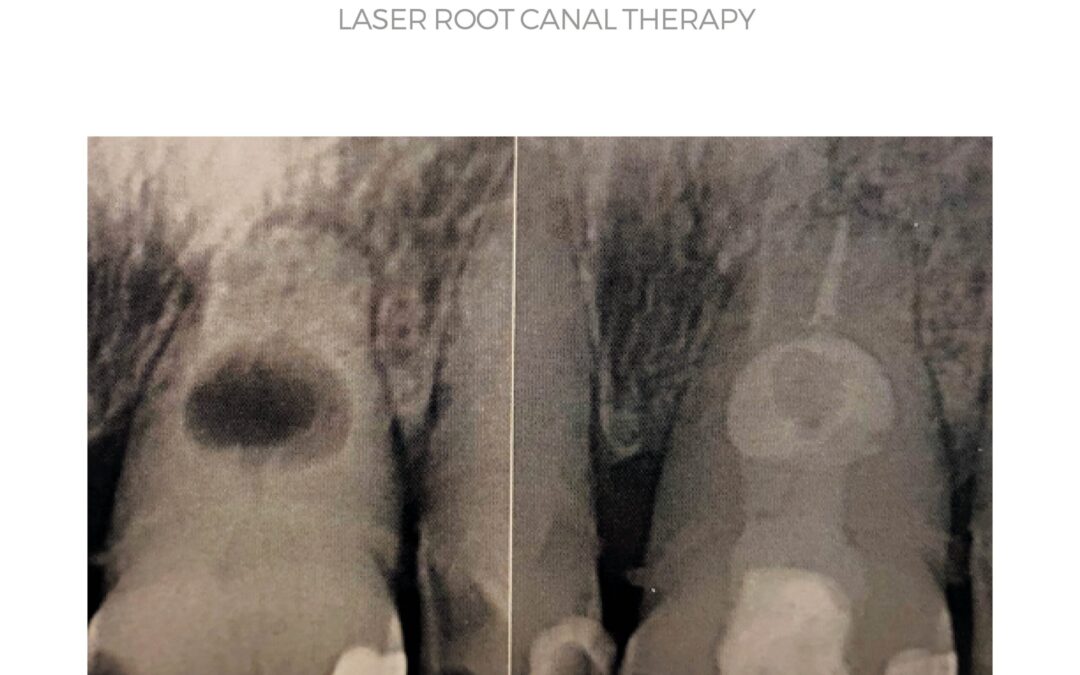
Popular culture often associates lasers with science-fiction weapons or real-life space exploration, but the technology can also be used inside the human body. At the Phoenix Endodontic Group, our endodontists frequently use laser-based tools to assist in root canal treatments.
The practice uses laser technology manufactured by Fontana (SSP and SWEEPS®) and Biolase (Waterlase) at its Phoenix office location. Both brands of tools provide extra assistance in the critical phases of cleaning and disinfecting tooth roots during a root canal treatment.
 Lasers Bring Benefits During A Root Canal Treatment
Lasers Bring Benefits During A Root Canal Treatment
-
The laser can provide initial cleaning in the coronal (crown) area of the tooth. An endodontist will begin a root canal by creating an opening in the crown. The laser can be used in this area of the tooth to remove calcifications and biological debris.
-
The laser can assist cleaning of the root canals. After a canal has been prepared using files or other tools, the endodontist may flood the canal with water and activate the laser while withdrawing the water from the space. The laser creates vapor bubbles, which collapse to form microbubbles and a pressure wave; these phenomena are what clean biofilm from the canals.
-
Laser treatment can also help disinfect the canals as they are being irrigated. Once the endodontist shapes the canals with their files, they will irrigate them with disinfecting liquids. Lasers can be used at this point to augment the disinfection process, with the pressure wave created by the vapor bubbles pushing the disinfectant deep into the canal recesses and generally making the process more effective than the traditional disinfecting step by itself.
-
Finally, lasers can be used to remove the chemical disinfectants prior to filling the canals. After the canals have been cleansed, shaped and disinfected, the laser tool can be used to remove the disinfecting liquid in the canals by activating it for about 30 seconds to vaporize any remaining liquid.
According to Dr. Jacqueline S. Allen, who practices at the Phoenix Endodontic Group, “One significant advantage to using lasers during root canals is that they can provide a more thorough removal of bacteria, debris and other materials without the risk of apical (tooth root area) extrusion.” She continues, “We are happy to explain to patients how we use Fontana and Biolase laser technology to enhance the safety and effectiveness of their root canal treatments.”






 The Key Stages Of Root Canal Therapy
The Key Stages Of Root Canal Therapy